What Is Degenerative Disc Disease All About?
Is it Really a Disease?
Sherwin Nicholson | Updated May 6, 2020
Don’t get too worried, just be concerned.
Although it is termed as a disease, degenerative disc disease (DDD) is not actually a disease. It is a natural process in which the condition of your discs gradually wears naturally over time.
It’s part of our aging process, and what we do (or don’t do for that matter) can accelerate (or minimize) it. The process is a very slow and steady one. Unfortunately, unless you have exceptional genes, it happens to everyone.
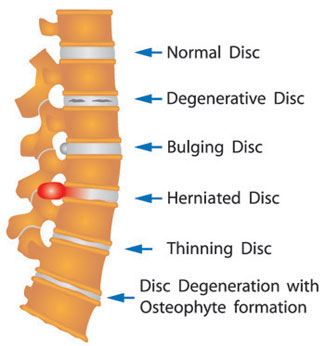
With this ‘disease’, the discs of your spine slowly become smaller in size and denser as the internal water composition decreases.
The Complications of DDD
As this happens, there is less protective cushioning when force is applied to them. The discs lose their original height resulting in the neighbouring vertebrae coming closer together.
As the vertebrae come closer together and the discs become thinner, there is less available flexibility of the spine.
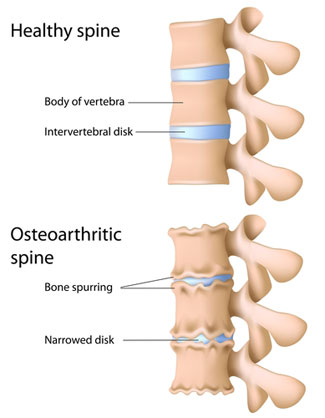
With age, you then become less able to bend your spine naturally. When you do bend your spine, the edges of the vertebrae are much more likely to touch. It is not a safe movement as there are increased risks of bone damage and the potential for osteophyte formation.
Progressive Wear with Aging
This disease affects everyone from about age 30 and above. When you are in your 60’s to 70’s it has significantly progressed to the point of causing chronic lower back pain. The rate of thinning can be accelerated if there is a history of pain, back injuries and disc herniations.
Lifestyle factors that add to DDD
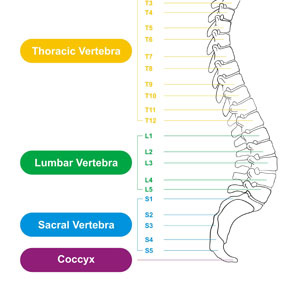
A lifestyle which includes heavy and repetitive lifting, physically demanding sports or even chronic sitting with poor posture make these discs prone to both rupture and thinning. The most common region of the spine to first wear are the lowest in position. The wear usually begins with the L5-S1 disc.
When you begin to feel the effects of the wear and tear that comes with DDD, there is a really good chance that your L5-S1 is involved.
Your L5-S1 Lumbar Disc, Herniations and Your Facet Joints
The L5-S1 is normally the largest but it also the most important, but used and abused. It connects your lumbar spine with your pelvis. It must bear the full weight and torque of the upper body under all conditions.
Therefore it is very common to have symptoms of lower back pain which involve this disc. It sustains the most torque and pressure anywhere up to 70% of the general load that the upper body bears.
The discs above, such as the L4-L5 and L3-L4 are generally the next in succession to wear and also in tandem with the L5-S1. These must then assume the tasks and abuse that the L5-S1 is no longer able to bear.
Doing everything possible to preserve your L5-S1 for as long as you can will make all the difference in the world for your safety.
Each of these discs provide less overall flexibility vertically as the lower ones become progressively more worn.
A herniation is not very easy to detect as immediate pain is first sensed. Thinning is very slow and sometimes undetectable until the it has progressed too far to treat properly.
When the discs have thinned excessively, there is likely to be nerve root impingement on the nerves that immediately exit from the vertebral space that they occupy.
Symptoms may include discomfort but will also include a slight numbness or tingling sensations running down the leg or thigh to the foot. Motor function may also be affected.
The facet joints are very prone to wear when disc height is compromised. As the vertebrae sit closer together, so do the facet joints. They bear more of the load as the height is lost. The cushions within the joint capsule of the facet joints themselves also begin to wear. Facet joints have a rich nervous supply and will also show signs of pain when irritated from wear.
Possible Remedies
There are many ways to correct or slow down this degenerative process. It is very unlikely that disc height will ever be restored. There is decompression therapy that claims to have successful results but it is not for everyone. With this type of treatment there is no fool proof guarantee in the long run that the discs will still be able to maintain any restored height.
Tips for Degenerative Disc Disease
Some general tips to reduce or limit the progression of degeneration are:
- Hydration – Drinking sufficient water to rehydrate the discs
- Correct posture to prevent disc imbalance
- Traction therapy/exercises to help restore height or volume
- Exercise and stretching to relieve tension and imbalances
- Sufficient sleep to help rehydrate the discs overnight
- Avoiding or minimizing heavy lifting
- Weight loss to reduce disc load
- Relaxation techniques to reduce tension in the lower back
We ALL develop DDD sooner or later
It is common to have DDD and no symptoms of lower back pain. The pain is usually from pressure on the adjacent nerves, rupture and facet joints inflammation. Mechanical, muscular discomfort is common with these conditions, so by correcting these problems you can alleviate a very large contributor to your pain.
DDD can also become worsened from the bad habits we have learned. This includes extended sitting, repetitively leaning over, lifting improperly, relying solely on painkillers and more.
For More Help with DDD:
Degenerative discs and the problems of sleep
Strengthen your abs to reduce DDD pain
A Downloadable guide to help you manage your DDD
References:
- U.S. National Library of Medicine 8600 Rockville Pike, Bethesda, MD 20894 U.S. Department of Health and Human Services National Institutes of Health https://medlineplus.gov/bp.html#cat93
- Intervertebral Disk Degeneration and Repair – James Dowdell, MD Mark Erwin, MD Theodoe Choma, MD Alexander Vaccaro, MD, PhD James Iatridis, PhD Samuel K. Cho, MD Neurosurgery (2017) 80 (3S): S46-S54. DOI: https://doi.org/10.1093/neuros/nyw078 Published: 21 February 2017
- Spinal stenosis-http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001477/
- Herniated disc/Slipped Disk-http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001478/
