When You Should See a Specialist For Back Pain
Depending on your symptoms, you may need to consult your doctor for a specialist sooner than later
by Sherwin Nicholson | Updated May 8, 2020
Getting help online is a common way of looking after your health, but don’t use it as your sole method for treatment.
I have listed some important areas you should be looking out for when it comes to back issues. They’ll help decide whether or not you may need specialized care.
You can learn the 3 health conditions you might misinterpret as simple back pain
Please consult with your family physician if you have any of the following 4 symptoms:
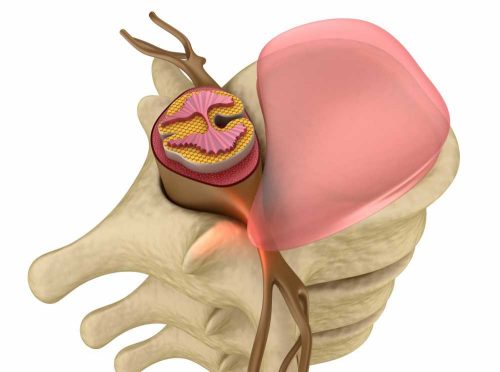
- A sharp, stabbing or severe pain in any region of your spine from head to buttocks. Symptoms are most common in the lumbar area of the spine and often more intense.
- Any symptoms of tingling or numbness. Often on one side of your body and down one or both legs.
- Whenever an extremity such as your leg exhibits sensations of BOTH weakness and discomfort.
- You have tiredness and weakness when walking even for a short distance.
The above symptoms may involve disc injury and nerve impingement which may require you to get an x-ray or MRI. Make an appointment to see your doctor as self-treatment shouldn’t be the first thing for you right now.
Don’t ignore the above symptoms as you could risk causing more injury for yourself. It’s all too common to put off or avoid proper treatment.
3 health conditions you might misinterpret as simple back pain
These conditions themselves can be pretty serious so be sure to get help if you think you may have one.
- Severe deficiency in vitamin D, calcium and magnesium mineral – If you have persistent issues of back muscle cramps especially while sleeping, it may be enough for you to try supplementation first. Your physician can also provide treatment for this condition.
- Restless leg syndrome – You feel the uncontrollable need to stay awake and away from bed at night due to leg discomfort – treatments are available, but a physicians’ consultation is required.
- Leg discomfort (including calf muscle cramps) that becomes worse after walking. We mistake these symptoms as being symptomatic of lumbar issues, but it’s actually vascular instead. Known as peripheral vascular disease, this requires urgent attention of a physician and possible referral to a vascular surgeon.
The most common form of back pain
If you want to know if your discomfort is better managed with either a therapist or by yourself, check out the following possible symptoms:
- Your level of discomfort varies over time. That is, it starts off worse in the morning and becomes more manageable later in the day.
- It is consistently interfering with your sleeping and morning routine. Translation: It always returns regardless of what you try to do to prevent it from happening.
- The symptom becomes easier to manage with more activity or exercise (less noticeable), but after resting, it returns. Sometimes even worse than before. It is common to believe that your form of exercise is helping to relieve you, but in cases where the pain gets worse post activity, you are NOT performing the right type or level of exercise(s).
- Symptoms of stiffness require anti-inflammatory if painkiller medication or go away with activity to relief, but only lasts for that duration. It is common for your stiffness to become even worse as you try to rely on rest to help control your stiffness.
- You have a clear and definite pattern where the symptom cycles from moderate/severe to little/no pain and over again. The morning or a rest period is where pain symptoms are most often your worst times.
- There are periods where you have good days, but your back suddenly gives out. Even though you may believe that you have an acute episode, this is a chronic condition that your body is experiencing.
- Your overall quality of life including the more rewarding activities are affected. Your schedule has been dependent upon pain management.
What you should do when these symptoms are because of your back
In virtually all cases, you are dealing with:
- muscle imbalances
- compromised joint mobility from these imbalances
- muscle and joint pain that varies with activity
- episodes that become better or worse because of these above three conditions
Step 1: Stop using the same methods of treatment as they are only temporary. Although easier said than done, what may seem like pain management at the time is negatively contributing to your condition.
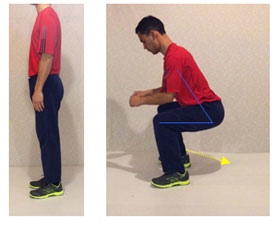
Step 2: Adopt safer ways to lift, move, twist, sit, etc. Avoid the weekend warrior lifestyle, especially when you get older. Learn how to reach down or lower yourself carefully to protect your spine.
Step 3: Follow recommended exercises, movements, and stretches that are protective and are intended to make your quality of life safer and easier.
General sports activities and conventional stretching methods may not be suitable unless they are protective.
Step 4: Follow highly recommended treatments that are unique only to your lumbar spine and avoid generalized fitness plans that may or may not be relevant to your condition. They could turn out to be the source of your condition.
Avoiding fitness programs does not mean that you should quit doing what you love to do. You may have to put the activity on hold or modify it to be safer.
These recommended steps are known to relieve your lower back. With both these above steps and by addressing these problem areas, your chances of living a pain-free lifestyle will be much better.
If you liked this article, you’ll also like:
6 Common Doctor-Recommended Remedies for Lower Back
4 Popular Treatments for Lower Back Pain
References: